You’re standing in front of the bathroom mirror, frustrated and confused. Your skin is red, irritated, and driving you crazy – but what exactly are you dealing with? If you’re like most of my patients, you’ve probably spent hours googling symptoms, trying to figure out whether that angry-looking rash is rosacea, eczema, or hives.
Here’s the thing: these three conditions love to masquerade as each other. I see patients every week at OC MedDerm in Irvine, CA, who’ve been treating the wrong condition for months because they look so similar. But once you know what to look for, the differences become much clearer.
Let me walk you through exactly how to tell them apart, what’s causing your skin to act up, and most importantly – what you can do about it.
Why Your Skin Keeps Getting Confused for Something Else
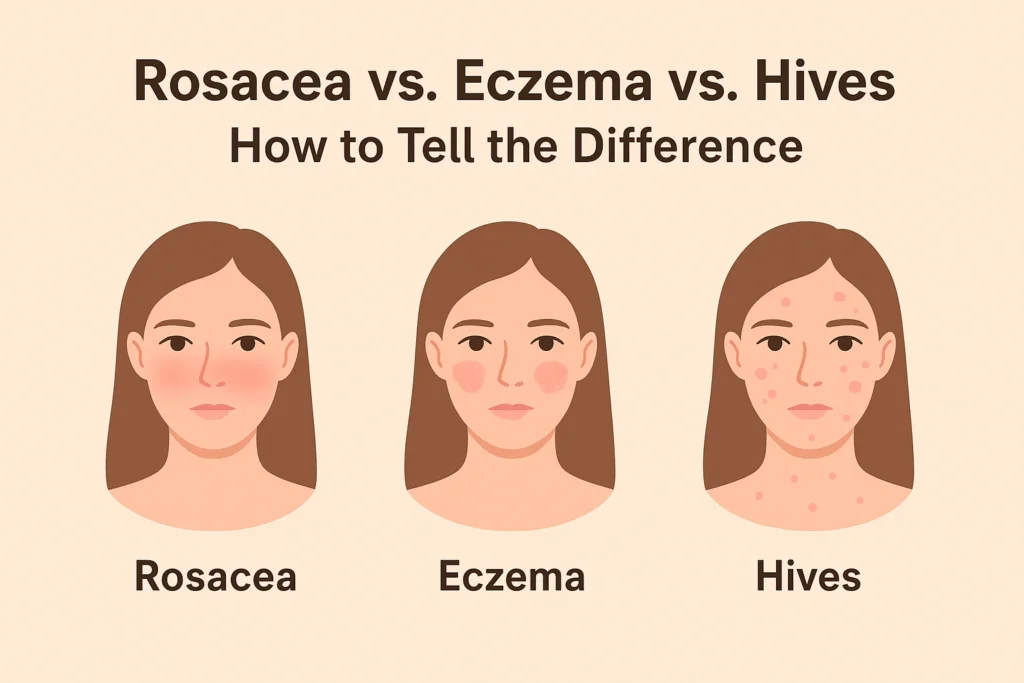
Before we dive into the specifics, let’s talk about why these conditions are such master impersonators. Eczema and rosacea are two of the most common chronic inflammatory skin conditions in the U.S. These disorders both cause red, irritated skin – and hives can throw another curveball into the mix with their own version of red, raised irritation.
The confusion is completely understandable. All three can make your skin look angry, feel uncomfortable, and leave you wondering if you’re using the wrong skincare products or if there’s something more serious going on.
But here’s what I want you to remember: getting the right diagnosis isn’t just about satisfying your curiosity. Each condition needs a completely different treatment approach. Using rosacea treatments on eczema (or vice versa) can actually make things worse.
The Tell-Tale Signs: How to Spot Each Condition
Rosacea: The Face-Focused Troublemaker
Rosacea is a common skin condition that causes redness and bumps on your face, most often on your nose, cheeks and forehead. If I had to pick one key identifier for rosacea, it’s location, location, location.
Rosacea has a very specific calling card – it loves the center of your face. Rosacea is typically localised to the centre of the face, particularly around the nose, whereas eczema can occur anywhere on the body. We’re talking about your nose, cheeks, forehead, and chin. It’s usually symmetrical too, so if your left cheek is red, your right cheek probably is too.
Here’s what rosacea looks like when it shows up:
The redness never really goes away. Unlike a temporary flush from exercise or embarrassment, rosacea gives you persistent redness that sticks around. Some of my patients describe it as looking like they have a permanent sunburn on the center of their face.
You might see tiny blood vessels. These spider-like vessels (we call them telangiectasias) become visible through your skin, especially on your nose and cheeks.
Bumps that aren’t quite pimples. Rosacea can create papules and pustules that look similar to acne, but they’re not the same thing. They tend to be more tender and don’t respond to typical acne treatments.
Your eyes might get involved. About half of people with rosacea also experience eye symptoms – redness, dryness, or a gritty feeling.
Eczema: The Itchy Overachiever
If rosacea is the face-focused condition, eczema is the overachiever that can show up literally anywhere on your body. Eczema usually causes dry, itchy, and scaly skin patches that last for a few days, but honestly, it can stick around much longer than that.
The hallmark of eczema is the itch. I’m not talking about a mild irritation – I’m talking about the kind of itch that wakes you up at night and makes you want to scratch until you bleed.
Here’s how to recognize eczema:
It loves skin folds. Eczema has favorite hangout spots – the insides of your elbows, behind your knees, on your wrists, and around your neck. On the face, it often appears around the eyes and mouth.
The skin looks dry and scaly. While rosacea tends to look flushed and inflamed, eczema often makes your skin look like it desperately needs moisture. It can appear thick, leathery, or flaky.
It comes and goes in flares. Eczema isn’t usually a constant presence like rosacea. It tends to flare up for days or weeks, then calm down, then flare again.
It can weep or crust over. In severe cases, eczema patches might develop small blisters that break open and form crusts – something you don’t typically see with rosacea.
Hives: The Quick-Change Artist
Now, hives are the wild card in this trio. Unlike the chronicity associated with eczema, hives are characterized by their transient nature, with raised red welts appearing and disappearing within hours.
If you’re dealing with hives, here’s what you’ll notice:
They appear suddenly and change quickly. You might wake up fine and by lunchtime have raised, red welts all over your arms. Or you might have a hive on your back that’s gone by evening but replaced by new ones on your legs.
They’re raised and often round or oval. Urticaria, or hives, presents as red, swollen welts that can quickly emerge and vanish across various body areas. These aren’t flat red patches – they’re raised bumps that you can feel with your finger.
They can appear anywhere. Unlike rosacea’s face preference or eczema’s love for skin folds, hives don’t discriminate. They can pop up anywhere on your body.
They’re usually very itchy. The itch from hives is different from eczema – it’s more of an immediate, urgent sensation rather than the chronic, gnawing itch of eczema.
What’s Actually Causing Your Skin to Act Up?
Understanding what triggers each condition can help you not only identify what you’re dealing with but also prevent future flare-ups.
Rosacea Triggers: The Usual Suspects
Rosacea triggers are surprisingly personal – what sets off your neighbor’s rosacea might not affect you at all. But there are some common culprits I see over and over:
Sun exposure is the biggest trigger for most people. Even brief exposure can cause a flare that lasts for days.
Heat in any form – hot showers, saunas, hot beverages, or even just a warm day can trigger flushing.
Spicy foods and alcohol are notorious for causing rosacea flares. Red wine is particularly problematic for many patients.
Stress can absolutely trigger rosacea. I’ve had patients whose rosacea flares every time they have a big presentation at work.
Certain skincare ingredients can be problematic. Fragrances, alcohol-based toners, and harsh exfoliants are common offenders.
Eczema Triggers: It’s Complicated
Eczema triggers are often a combination of internal and external factors:
Genetics play a huge role. If your parents had eczema, asthma, or seasonal allergies, you’re more likely to develop eczema too.
Environmental allergens like dust mites, pet dander, pollen, or mold can trigger flares.
Irritants including harsh soaps, detergents, fragrances, and even certain fabrics can cause problems.
Food allergies sometimes play a role, especially in children. Common culprits include milk, eggs, nuts, and soy.
Stress and hormonal changes can definitely trigger eczema flares.
Weather changes – both very dry conditions and excessive humidity can be problematic.
Hives Triggers: The Allergy Connection
They frequently develop from an allergic reaction to food, medicine, or other allergens and might appear unexpectedly.
Food allergies are a major cause. Shellfish, nuts, eggs, and dairy are common culprits, but any food can potentially cause hives.
Medications – antibiotics, pain relievers, and blood pressure medications are frequent causes.
Physical triggers like pressure from tight clothing, temperature changes, sunlight, or even exercise can cause hives in some people.
Infections – viral infections, in particular, can trigger hives, especially in children.
Stress can absolutely cause hives, though it’s often a combination of stress plus another trigger.
The Diagnosis Dilemma: Why You Need Professional Help
Here’s something that might surprise you: Rosacea is sometimes confused with other conditions because its signs and symptoms can appear so similar, and a diagnosis by a dermatologist is essential.
Even as a dermatologist with years of experience, I sometimes need to take a careful history, examine the skin closely, and occasionally run tests to make the right diagnosis. Self-diagnosis based on internet photos can lead you down the wrong treatment path for months.
I had a patient recently who was convinced she had rosacea because her cheeks were always red. She’d been using gentle, fragrance-free products and avoiding all her favorite spicy foods for six months. When I examined her, it was clear she actually had eczema – and she’d been avoiding treatments that could have helped her while restricting her diet unnecessarily.
When You Absolutely Need to See a Doctor
Some situations require immediate professional attention:
If hives are accompanied by difficulty breathing, swallowing problems, or facial swelling – this could be anaphylaxis, which is a medical emergency.
If you have widespread, severe eczema that’s interfering with your sleep or daily activities.
If your skin shows signs of infection – increased warmth, pus, red streaking, or fever.
If over-the-counter treatments aren’t helping after a few weeks.
If you’re not sure what you’re dealing with – better to get it right from the start than waste time and money on the wrong treatments.
Treatment Approaches: What Actually Works
The frustrating truth is that there’s no one-size-fits-all treatment for any of these conditions. What works depends on your specific triggers, the severity of your symptoms, and how your skin responds to different approaches.
Rosacea Treatment: Gentle but Persistent
For rosacea, we focus on reducing inflammation and avoiding triggers:
Topical treatments like metronidazole gel are often first-line treatments. These prescription medications can significantly reduce redness and bumps over time.
Oral antibiotics might be necessary for moderate to severe cases. We use them more for their anti-inflammatory properties than their antibiotic effects.
Laser and light therapies can be incredibly effective for reducing visible blood vessels and persistent redness.
Gentle skincare is crucial. I recommend mineral sunscreen daily, fragrance-free cleansers, and moisturizers designed for sensitive skin.
Eczema Treatment: Moisture and Management
Eczema treatment is all about restoring the skin barrier and controlling inflammation:
Moisturizing is non-negotiable. I tell patients to apply a thick, fragrance-free moisturizer while their skin is still damp from showering.
Topical corticosteroids are often necessary during flares to reduce inflammation and itching.
Prescription non-steroidal options like calcineurin inhibitors can be great for sensitive areas like the face.
Identifying and avoiding triggers is crucial for long-term management.
For severe cases, we have newer biological treatments that can be life-changing for people who haven’t responded to other therapies.
Hives Treatment: Stop the Reaction
Antihistamines are typically effective for relief. For hives, the approach depends on whether they’re acute or chronic:
Antihistamines are the first line of defense. Both over-the-counter and prescription options can be effective.
Avoiding known triggers is essential, though sometimes we need to do detective work to figure out what those triggers are.
For chronic hives, we might need stronger medications like oral corticosteroids or other immune-modulating treatments.
Cool compresses and loose clothing can provide comfort during flares.
Your Daily Management Strategy
Regardless of which condition you’re dealing with, there are some universal principles that can help:
The Universal Skincare Rules
Less is more. Complicated skincare routines with multiple active ingredients are often more harmful than helpful for irritated skin.
Fragrance-free everything. This includes your laundry detergent, soap, shampoo, and skincare products.
Lukewarm water only. Hot water strips your skin’s natural oils and can trigger flares in all three conditions.
Pat, don’t rub. Whether you’re drying off after a shower or applying moisturizer, gentle patting motions are less irritating than rubbing.
The Trigger Detective Work
Start keeping a simple diary of your symptoms. Note:
- What your skin looked like when you woke up
- Any new products you used
- What you ate
- Stress levels
- Weather conditions
- How your skin looked at bedtime
After a few weeks, patterns often emerge that can help you identify your personal triggers.
The Stress Connection
All three conditions can be worsened by stress, and having a skin condition is inherently stressful – it’s a frustrating cycle. Finding healthy ways to manage stress (exercise, meditation, therapy, hobbies) isn’t just good for your mental health; it’s good for your skin too.
What Not to Do: Common Mistakes That Make Things Worse
In my years of practice, I’ve seen patients make the same mistakes over and over. Here are the big ones to avoid:
Don’t try to treat suspected rosacea with acne products. Benzoyl peroxide and salicylic acid can make rosacea significantly worse.
Don’t over-moisturize eczema with heavy, greasy products. While moisturizing is crucial, using products that are too heavy can sometimes trap heat and make itching worse.
Don’t ignore chronic hives. If you’re getting hives regularly for more than six weeks, there might be an underlying cause that needs investigation.
Don’t rely on home remedies without medical guidance. Essential oils, DIY masks, and internet cure-alls can often make skin conditions worse.
Don’t stop treatment too early. Many of these conditions require consistent, long-term management. Stopping treatment as soon as you see improvement often leads to rebound flares.
When to Worry: Red Flags That Need Immediate Attention
Most skin conditions are frustrating rather than dangerous, but there are some warning signs that require urgent medical attention:
- Difficulty breathing or swallowing (especially with hives)
- Facial swelling, particularly around the eyes or mouth
- Signs of skin infection (pus, red streaking, fever)
- Severe, widespread rash that appears suddenly
- Any skin condition that’s interfering significantly with your sleep or daily activities
The Bottom Line: You Don’t Have to Suffer
Here’s what I want you to remember: chronic skin conditions are incredibly common, they’re not your fault, and they’re definitely treatable. According to the American College of Allergy, Asthma and Immunology, 20% of people will experience hives at some point in their lives. You’re not alone in dealing with these frustrating skin issues.
The key is getting the right diagnosis and the right treatment plan. What works for your friend’s eczema might not work for your rosacea. What cleared up your hives last time might not be the right approach if they come back.
Don’t spend months or years being frustrated with treatments that aren’t working. Professional evaluation can save you time, money, and a lot of unnecessary discomfort.
Ready to Get Answers About Your Skin?
If you’re tired of playing the guessing game with your skin condition, it’s time to get some professional insight. Every day you wait is another day of potential discomfort and possibly using the wrong treatments.
I’ve seen countless patients find relief once they finally got the right diagnosis and treatment plan. Whether you’re dealing with the persistent redness of rosacea, the maddening itch of eczema, or the unpredictable nature of hives, there are effective treatments available.
Don’t let uncertainty keep you from getting the help you need. Schedule a consultation today and let’s figure out exactly what’s going on with your skin – and more importantly, how to fix it.
Ready to stop guessing and start getting results? Contact us at +1(949) 551-1113 or visit to schedule your appointment at OC MedDerm in Irvine, Orange County, CA. Your skin deserves expert care, and you deserve to feel confident and comfortable again.
No comments:
Post a Comment